- Anatomical terminology
- Skeletal system
- Joints
- Muscles
- Heart
- Blood vessels
- Lymphatic system
- Nervous system
- Respiratory system
- Digestive system
- Urinary system
- Female reproductive system
- Male reproductive system
- Endocrine glands
- Eye
- Ear
Pancreas
The pancreas (Latin: pancreas) is an organ located in the back of the abdomen behind the stomach. It is a part of two organ systems - the digestive and endocrine systems. The pancreas is a gland that consists of exocrine and endocrine parts. Its exocrine function is aiding in digestion by producing enzymes that help break down fats, proteins and carbohydrates. The primary endocrine function of the pancreas is to produce hormones responsible for regulating blood sugar.
Pancreas anatomy
The pancreas is shaped like a flattened pear or a fish. It weighs approximately 60-100 grams; its length is around 12-15 cm, and thickness 2-3 cm. The longitudinal axis of the pancreas extends from the right side to the left side, from the bottom to the top. The gland is surrounded by other abdominal organs, including the small intestine, spleen, and liver. It is situated in the epigastric and hypochondriac regions of the abdomen. The peritoneum covers the pancreas only from the anterior aspect, meaning that the pancreas is located retroperitoneally.
The pancreas has two main ducts – pancreatic duct and accessory pancreatic duct. The pancreatic duct goes through the pancreas parallel to the longitudinal axis of the gland. It connects to the common bile duct in the posterior wall of the descending part of the duodenum. This connection creates an extension called the ampulla of Vater, which has a small opening - major duodenal papilla - that opens in the duodenum. The small opening is surrounded by the Oddi sphincter.
The Oddi sphincter is made from smooth muscles that regulate the flow of bile and pancreatic juices into the duodenum. The muscles relax when food passes into the duodenum. But when there is no food in the duodenum, the muscles contract, and the opening closes. Near the opening for the pancreatic duct there is an opening for the accessory pancreatic duct. It is called the minor duodenal papilla and it is found in the back wall of the duodenum. The accessory pancreatic duct releases pancreatic juices from the head of the pancreas.
Parts of pancreas
The pancreas has four parts:
- Head
- Uncinate process
- Neck
- Body
- Tail
Head of pancreas
The head of the pancreas is the widest part of the organ. This part of the pancreas is located within the curvature of the duodenum. The location is significant as this is also where the stomach comes into contact with the first part of the small intestine, meaning that this is where digestive enzymes are released from the pancreas through the major and minor duodenal papillae. The head of the pancreas is flat, therefore, it has only two surfaces: anterior surface and posterior surface.
The pancreatic head is situated at the level of the second lumbar vertebra (L2). It has an uncinate process that is a projection from the inferior part of the head. Anterior to the head of the pancreas are the peritoneum and the transverse colon, and the transverse mesocolon (a meso-fold of the peritoneum). Behind the pancreatic head sits the inferior vena cava, portal vein, and common bile duct. To the right, the left, and inferiorly the head of the pancreas is surrounded by the duodenum.
Neck of pancreas
The neck of the pancreas extends from the right upper part of the front of the pancreatic head. It is directed upwards and forwards. Then again upwards and continues as the body to the left. In front of the pancreatic neck lies pylorus of the stomach. Posteriorly to the neck are the superior mesenteric vessels. Also posteriorly, the superior mesenteric vein and the splenic vein connect to form the portal vein.
Body of pancreas
The body of the pancreas is the largest part of the gland. It lies behind the stomach and crosses the vertebral column.
The body of the pancreas has a triangular form with three surfaces and three borders:
- Anterosuperior surface
- Posterior surface
- Anteroinferior surface
- Superior border
- Inferior border
- Anterior border
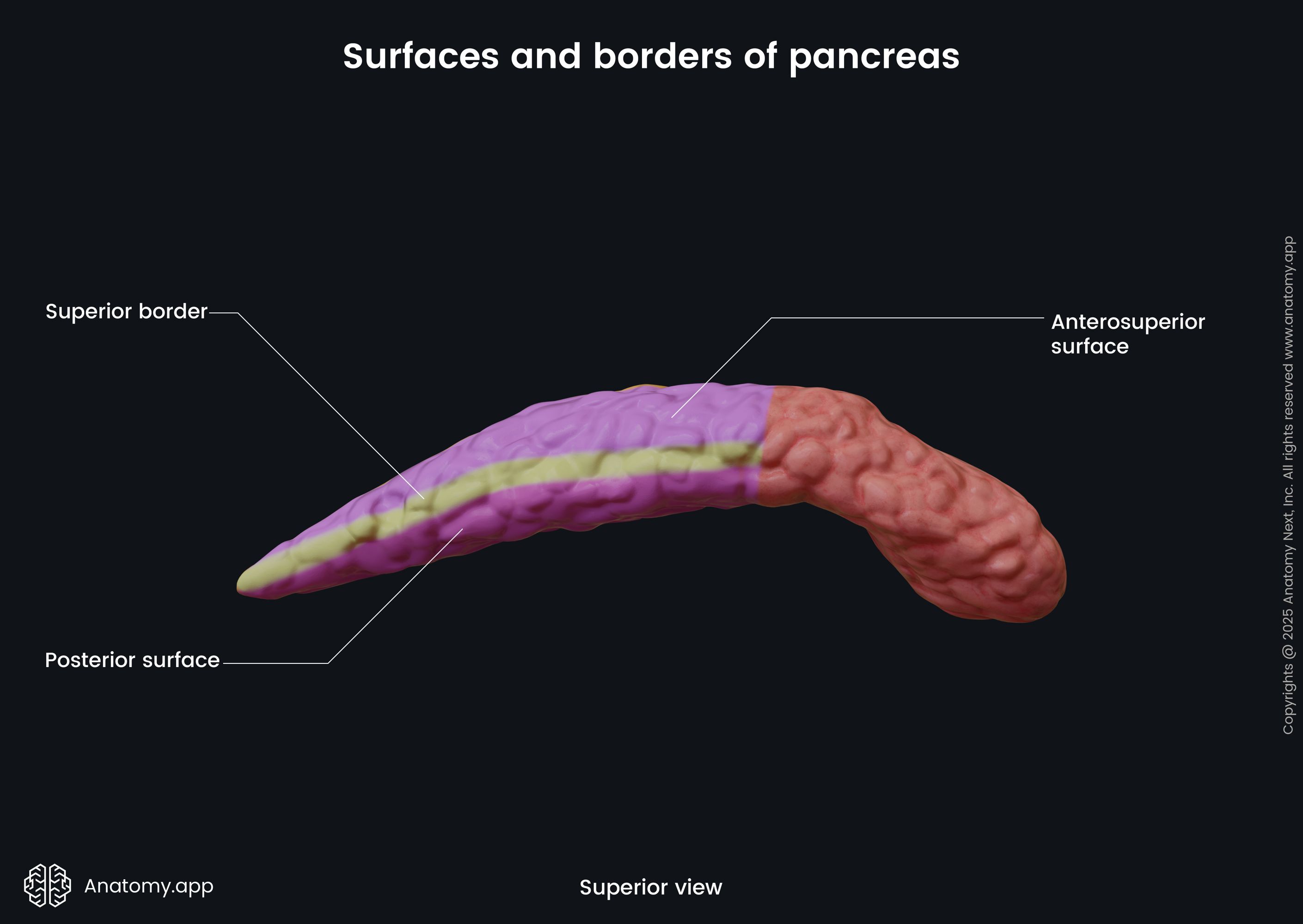
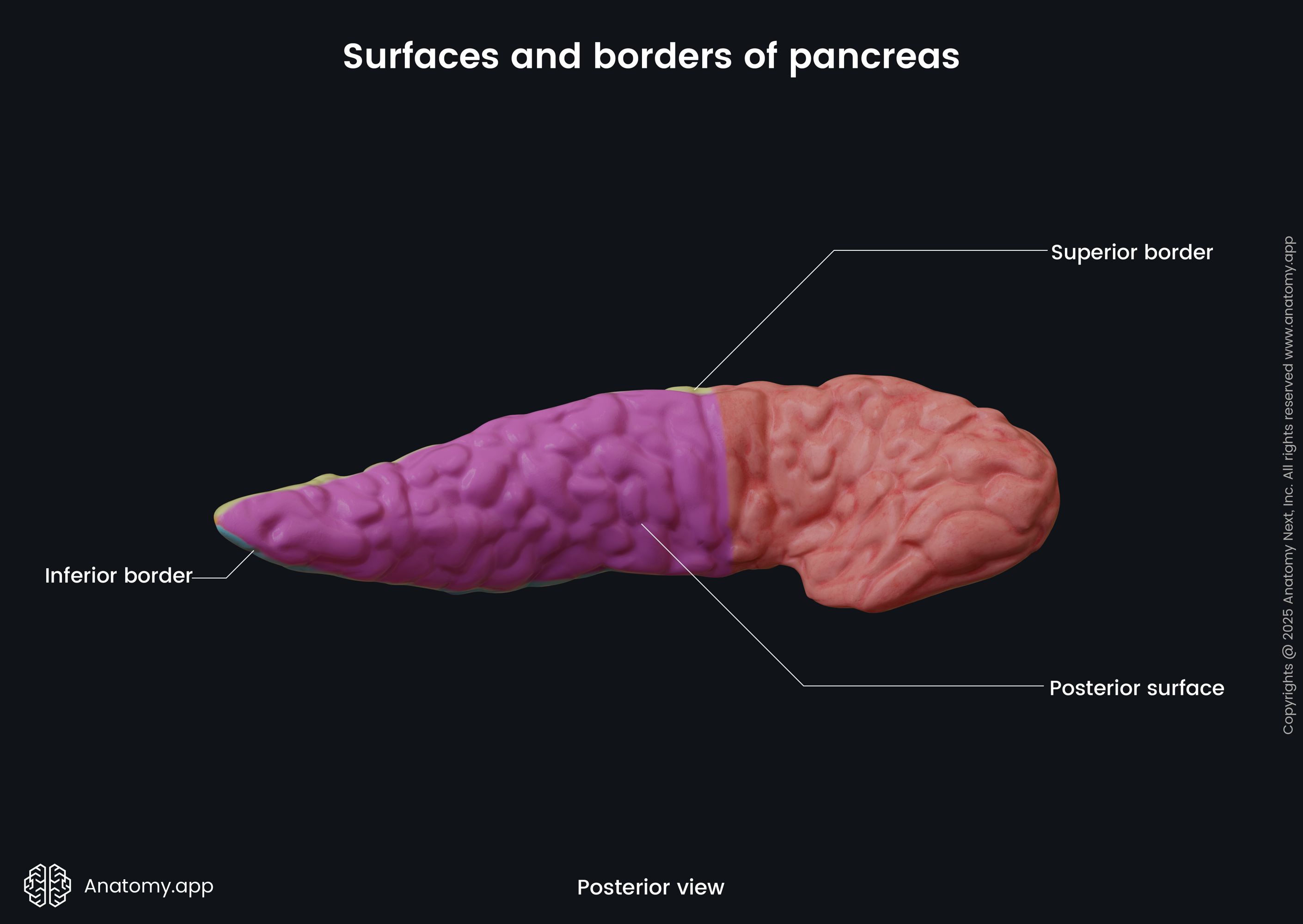
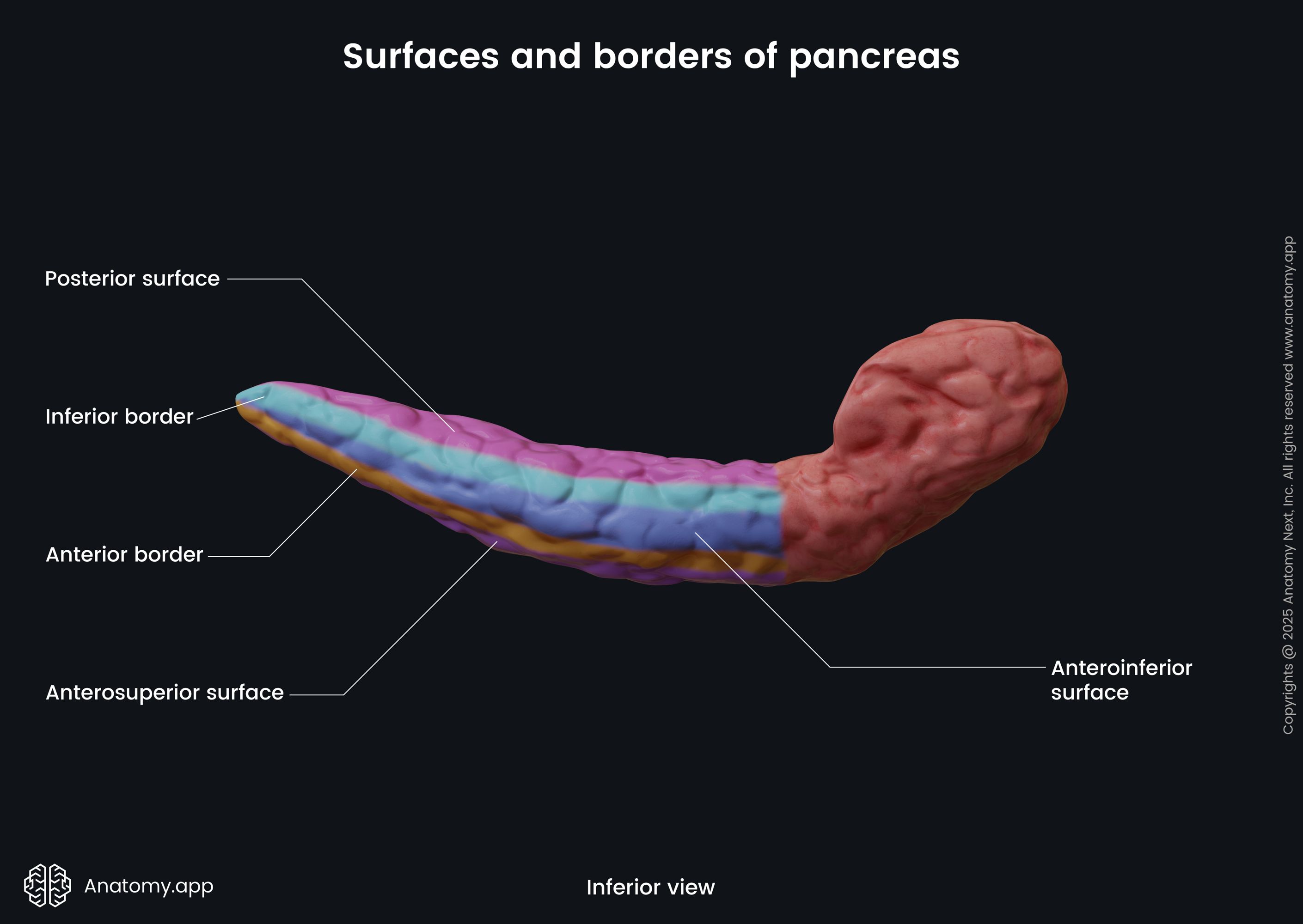
The body of the pancreas crosses the spine from the right to the left side at the level of the first lumbar vertebra (L1). In front of the pancreatic body lies the stomach and the transverse colon. Posteriorly to the body are the abdominal aorta, celiac plexus, splenic vein, left kidney with the left renal artery, as well as the initial part of the superior mesenteric artery. Below the body of the pancreas sits the duodenojejunal flexure, loops of the jejunum, and the left colic flexure. The splenic artery passes along the top of the superior margin, while next to the anterior margin lies the transverse mesocolon.
Tail of pancreas
The body of the pancreas without any particular border changes into the tail of the pancreas. Like the body, the tail of the pancreas also has a triangular shape with the same three surfaces and three margins. The tail ends at the level of the tenth rib. The tail of the pancreas lies between the layers of the splenorenal ligament. The same organs that surround the body of the pancreas mostly surround the tail.
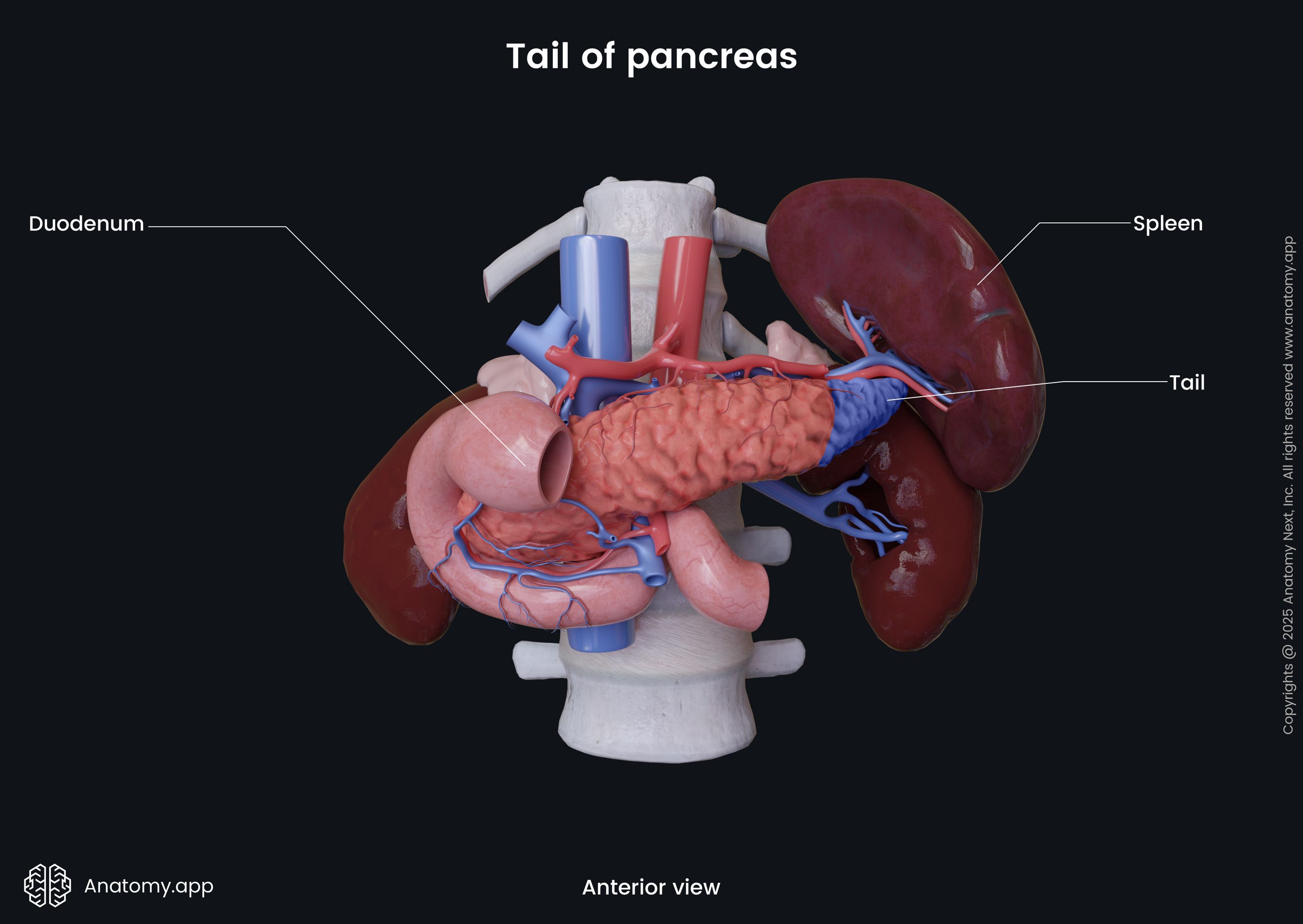
From the anterior side, there is the stomach and the transverse mesocolon. Behind the tail of the pancreas lies the abdominal aorta, celiac plexus, splenic vein, and left kidney. Inferiorly, sits the duodenojejunal flexure, jejunum loops, and left colic flexure. The splenic artery passes along its superior margin, and next to the anterior margin lies the transverse mesocolon. Laterally to the tail of the pancreas lies the hilum of the spleen.
Neurovascular supply of pancreas
The pancreas is an organ rich in blood supply. As the pancreas consists of both endocrine and exocrine glands, the innervation for both functional parts differs.
Arterial blood supply
The arterial blood supply of the pancreas is provided by vessels that originate from the celiac trunk and superior mesenteric artery. The celiac trunk gives rise to the splenic artery, which runs along the superior margin of the pancreas. This artery gives branches that supply the left part of the body and the tail of the pancreas. The most prominent pancreatic branch of the splenic artery is called the grater pancreatic artery.
The head of the pancreas is supplied by the superior and inferior pancreaticoduodenal arteries. They run along the posterior and anterior surfaces of the head of the pancreas. The superior and inferior pancreaticoduodenal arteries are branches of the gastroduodenal artery (a branch of the common hepatic artery that arises from the celiac trunk) and superior mesenteric artery, respectively. The pancreaticoduodenal arteries join to form an anastomosis in the middle.
Venous drainage
The venous blood from the body and tail of the pancreas is collected by the splenic vein. The head of the pancreas is drained by the pancreaticoduodenal veins that accompany the superior and inferior pancreaticoduodenal arteries and typically flow into the superior mesenteric vein and portal vein.
Lymphatic drainage
Lymph from the body and tail of the pancreas is drained to splenic lymph nodes and further to the lymph nodes in front of the aorta (periaortic lymph nodes). From the head of the pancreas, lymph is drained carried to the pyloric lymph nodes and eventually drained to the periaortic lymph nodes. From the periaortic lymph nodes, lymphatic vessels carry lymph to the superior mesenteric or celiac lymph nodes.
Innervation
The pancreas receives its involuntary innervation from the autonomic nervous system. The sympathetic innervation arises from the greater and lesser splanchnic nerves that originate from the T5 - T12 spinal cord segments. Its parasympathetic innervation comes from the vagus nerve (CN X), the tenth cranial nerve. Both parasympathetic and sympathetic fibers continue to the celiac ganglion and superior mesenteric plexus.
The acinar cells and the pancreatic islets inside of the pancreas also receive nerve signaling. The parasympathetic system incites secretion of pancreatic juice, insulin, and glucagon from acinar cells, while the sympathetic system is responsible for inhibition of pancreatic juice, exocrine secretion. At the same time, sympathetic fibers inhibit the release of insulin while stimulating the release of glucagon.
Pancreas histology
As the pancreas has both endocrine and exocrine functions, the cells of this organ can be divided based on their roles.
Exocrine part of pancreas
The majority of the pancreatic cells are responsible for the exocrine (digestive) function. The main cells are called acinar cells because they form clusters (acinus) around small ducts. The clusters form lobes that have fibrous walls. The acinar cells secrete digestive enzymes like trypsin and chymotrypsin to digest proteins, amylase to help digest carbohydrates, and lipase to break down fats.
The pancreatic enzymes are secreted through small ducts surrounding the acinar cells. The acinar cells have a pyramidal form and are located around the intercalated ducts. The intercalated ducts eventually merge and become intralobular ducts that drain into interlobular ducts. After draining through the system of ducts, the pancreatic juices end up in the pancreatic duct. In the ducts, cells are no longer pyramid-shaped; they are column-shaped and can be seen in more than one cell layer.
Endocrine part of pancreas
The endocrine function of the pancreas is provided by cells that form many clusters of cells - pancreatic islets, also known as islets of Langerhans. The different cell types forming the islets are known as alpha cells, beta cells, delta cells, gamma cells, and epsilon cells. Each cell group is responsible for a production of a specific hormone. Based on the hormones they produce, their location within the islets are also different.
- Alpha cells secrete glucagon and are located in the periphery of the islets, composing around 15-20% of all cells in the islets.
- Beta cells secrete insulin and are located throughout the islets; they are also increased in numbers compared to alpha cells, around 65-80%. Insulin and glucagon participate in regulating blood glucose levels.
- Delta cells are responsible for the release of somatostatin and are also located in the periphery of the islets, forming only 3-10% of all the cells in the islets.
- Only 3-5% of the cells in the islets are gamma cells. These cells produce pancreatic polypeptide, which regulates both endocrine and exocrine functions.
- The least represented cells in the islets are epsilon cells, which compose less than 1% of all cells in the islets and secrete ghrelin. Apart from other released hormones, ghrelin is a protein that stimulates sense of hunger.
Pancreatic islets have many small arterioles to receive blood supply for efficient secretion and venules for the hormones to drain into the circulation. The signaling way within the pancreatic islets is paracrine. The feedback system in the islets depends on the other islet cells and their produced hormones. After release, insulin activates other beta cells but inhibits alpha cells. Glucagon activates other alpha cells, then that process leads to the activation of beta cells and delta cells. And somatostatin inhibits other pancreatic cells.
Pancreas functions
The pancreas has two main functions: exocrine - aiding in digestion, and endocrine - regulation of blood sugar levels.
Exocrine function
The function of the pancreas in the digestive system is to help to break down food components. Acinar cells secrete enzymes that help digestion. As mentioned above, these enzymes are trypsin and chymotrypsin for digesting proteins, amylase for digesting carbohydrates, and lipase to break down fats. Pancreas enzymes are secreted as proenzymes that are inactive and are activated by enterokinase present in the duodenum.
The pancreatic enzymes are released through a duct system that ends with the pancreatic duct leaving the pancreas. The pancreatic duct joins with the common bile duct and forms the ampulla of Vater that opens in the duodenum. The pancreatic juices containing the enzymes are mixed with bile from the common bile duct, and this mix is released in the duodenum to help digest fats, proteins, and carbohydrates. 1.5-3 liters of secrete is produced by the pancreas every day.
Even though ghrelin and pancreatic polypeptide are secreted in the endocrine part of the pancreas (the pancreatic islets), they also take part in the digestive function. In contrast, somatostatin, also secreted by cells of the pancreatic islets, takes part in both processes. The role of somatostatin in the digestive system is to decrease gastric emptying rate by reducing smooth muscle contractions and blood flow within the intestines. The hormone also inhibits the secretion of pancreas enzymes.
Ghrelin, apart from other hormones stimulated from the islets, is a protein that stimulates hunger. Ghrelin is mostly produced in the stomach, but as mentioned before small amounts are also secreted by cells of the pancreatic islets. Ghrelin stimulates appetite leading to an increased food intake and fat storage. Ghrelin levels increase before eating and during fasting. After eating, ghrelin levels decrease. Somatostatin and other hormones released in the digestive tract inhibit release of ghrelin.
The release of pancreatic polypeptide is stimulated by eating, exercising, and fasting. It is released together with insulin, and acts upon both exocrine and endocrine cells. The pancreatic polypeptide participates in digestive processes, as it inhibits the secretion of pancreatic enzymes after a meal, while stimulating the secretion of gastric juice.
Endocrine function
The function of the pancreas within the endocrine system is to release hormones into the bloodstream, mainly to regulate blood glucose levels among other functions. Insulin and glucagon are the main hormones released from the endocrine parts of the pancreas - the pancreatic islets. These hormones are responsible for maintaining normal blood glucose levels. Change in blood glucose level is the initiator of producing these hormones.
When the blood glucose levels are low, it sends a signal to alpha cells in the islets to produce glucagon, which ultimately elevates the blood glucose level. Additionally, also low insulin levels and exercise can initiate the release of glucagon. Glucagon acts on the liver cell receptors and stimulates the liver to convert glycogen (that is stored in the liver) into glucose and to release glucose into the bloodstream, thus elevating the blood glucose level. This process is called glycogenolysis, as glycogen is being broken down.
When the liver's storage of glucose (in the form of glycogen) slowly empties, glucagon stimulates the liver and kidneys to make more glucose in a process called gluconeogenesis. At the same time, glucagon can shut off glycolysis in the liver and can induce lipolysis and glucose production from fat. Also, glucagon decreases the uptake of glucose in fatty cells and muscles to elevate the blood glucose level.
When the blood glucose levels are high, beta cells get activated, and they start to release insulin to decrease blood glucose level. The primary function of insulin is to change blood glucose into glycogen through a process called glycogenesis happening in the liver and muscle cells. Insulin works by stimulating cells to uptake glucose, especially skeletal muscle cells, which decreases the blood glucose level. Insulin also works as an inhibitory hormone to stop gluconeogenesis and promote the storage of glucose in fat by inhibiting lipolysis.
Not only blood glucose levels, insulin levels, and exercise affect the release of these hormones. Amino acids also can stimulate the release of insulin and glucagon. Somatostatin, which is secreted by delta cells in the islets, inhibits insulin and glucagon release. The release of somatostatin is stimulated by the beta cells of the pancreatic islets.
The sympathetic nervous system can also stimulate secretion of insulin and glucagon through activation of beta-2 receptors by catecholamines. And activation of alpha-1 receptors inhibits insulin and glucagon release from the pancreatic islets. stimulation of muscarinic acetylcholine receptors (M3) through the parasympathetic nervous system and the vagus nerve (CN X) stimulates insulin release from beta cells in the islets.
Pancreatic disorders
The pancreas may be affected by various pathologies, but the most common ones are diabetes, pancreatitis, and pancreatic cancer. Less common are islet cell tumors, cystic fibrosis, pancreatic cysts. Pancreatic problems may be difficult to notice early, especially cancer and tumors, which often do not present with specific symptoms in the early stages.
Some diseases of the pancreas can be noticed early and treated or controlled relatively easily, but can lead to life-threatening conditions if left untreated. Pancreatic cancer is known to be aggressive, diagnosed mostly in late stages, and with a low survival rate. As symptoms for many pancreatic diseases are general and unspecific, problems with the pancreas are often diagnosed late.
Pancreatitis
Pancreatitis refers to inflammation of the pancreas. It can be acute, chronic, or hereditary. Acute pancreatitis typically manifests as a sudden attack of pain in the upper abdomen. The pain usually is severe and can last for several days. The pain usually radiates to the back and can be described as belt-type pain. The pain typically worsens after eating. People can also have fever, nausea, vomiting, and tenderness when touching the abdomen.
Chronic pancreatitis is a progressive disease. The most commons signs of chronic pancreatitis are a pain in the upper abdomen and diarrhea. As the disease progresses, malnutrition and weight loss can be seen. If lead to late stages, pancreatitis can initiate the development of diabetes. The main risk factors and causes of pancreatitis are:
- Alcoholism
- Smoking
- Obesity
- Family history
- Injury to the abdomen
- Gallstones
- Pancreatic cancer
- Abdominal surgery
Diabetes
Diabetes is a chronic disorder that affects blood glucose levels. The most common types of diabetes are type 1, type 2, and gestational diabetes. The reason for type 1 diabetes is unknown but believed to be triggered by the body's own immune system (autoimmune process). In the case of type 1 diabetes, beta cells that produce insulin are attacked and destroyed by immune responses. What triggers the immune system to attach beta cells is still unknown, but it might be genetic and environmental factors. In type 1 diabetes, ultimately, there are no beta cells that could produce insulin, which the main difference from type 2 diabetes.
Type 2 diabetes is the most common type of diabetes. It can be caused by lifestyle, genes, and also polycystic ovarian syndrome in women. The main risk factors for type 2 diabetes are overweight, inactivity, family history, age, high blood pressure, too high cholesterol, and triglyceride levels. In this type of diabetes, the beta cells are not destroyed; they are still producing insulin, but the cells become insulin resistant. This means that liver, muscle and fat cells do not take up insulin efficiently enough, so the body needs help with this process, as with time pancreas cannot produce enough insulin.
Gestational diabetes is a type of diabetes that develops during pregnancy. It is connected to family history and insulin resistance that may happen due to weight gain during pregnancy. Many other diseases and medication can cause diabetes. Some common symptoms of diabetes are:
- Increased appetite
- Increased thirst
- Increased urination
- Fatigue
- Blurred vision
- Weight loss for no reason
- Sores that do not heal well
- Numbness in the palms or feet
Pancreatic cancer
Pancreatic cancer develops when malignant cells form in the pancreatic tissue. Pancreatic cancer is tricky as it may not have any specific early signs. The most common symptoms are jaundice, dark urine, light-colored stools, pain in the upper or middle part of the abdomen and back, weight loss for no reason, loss of appetite, tiredness. However, these symptoms only develop in late stages.
Therefore, pancreatic cancer is difficult to detect. Pancreatic cancer is rarely found in early stages because of the lack of specific symptoms. If it is found early, pancreatic cancer can be cured by surgical resection. If pancreatic cancer is diagnosed in late stages, the treatment is only palliative to improve the quality of life and treat symptoms. Risk factors for pancreatic cancer include the following:
- Obesity
- Smoking
- Lack of physical activities
- Diabetes or chronic pancreatitis in history
- Family history of pancreatic cancer or pancreatitis
- Certain hereditary diseases, such as:
- Von Hippel-Lindau syndrome
- Hereditary breast and ovarian cancer syndrome
- Lynch syndrome
- Multiple endocrine neoplasia type 1 syndrome