- Anatomical terminology
- Skeletal system
- Joints
- Muscles
- Heart
- Blood vessels
- Lymphatic system
- Nervous system
- Respiratory system
- Digestive system
- Urinary system
- Female reproductive system
- Male reproductive system
- Endocrine glands
- Eye
- Ear
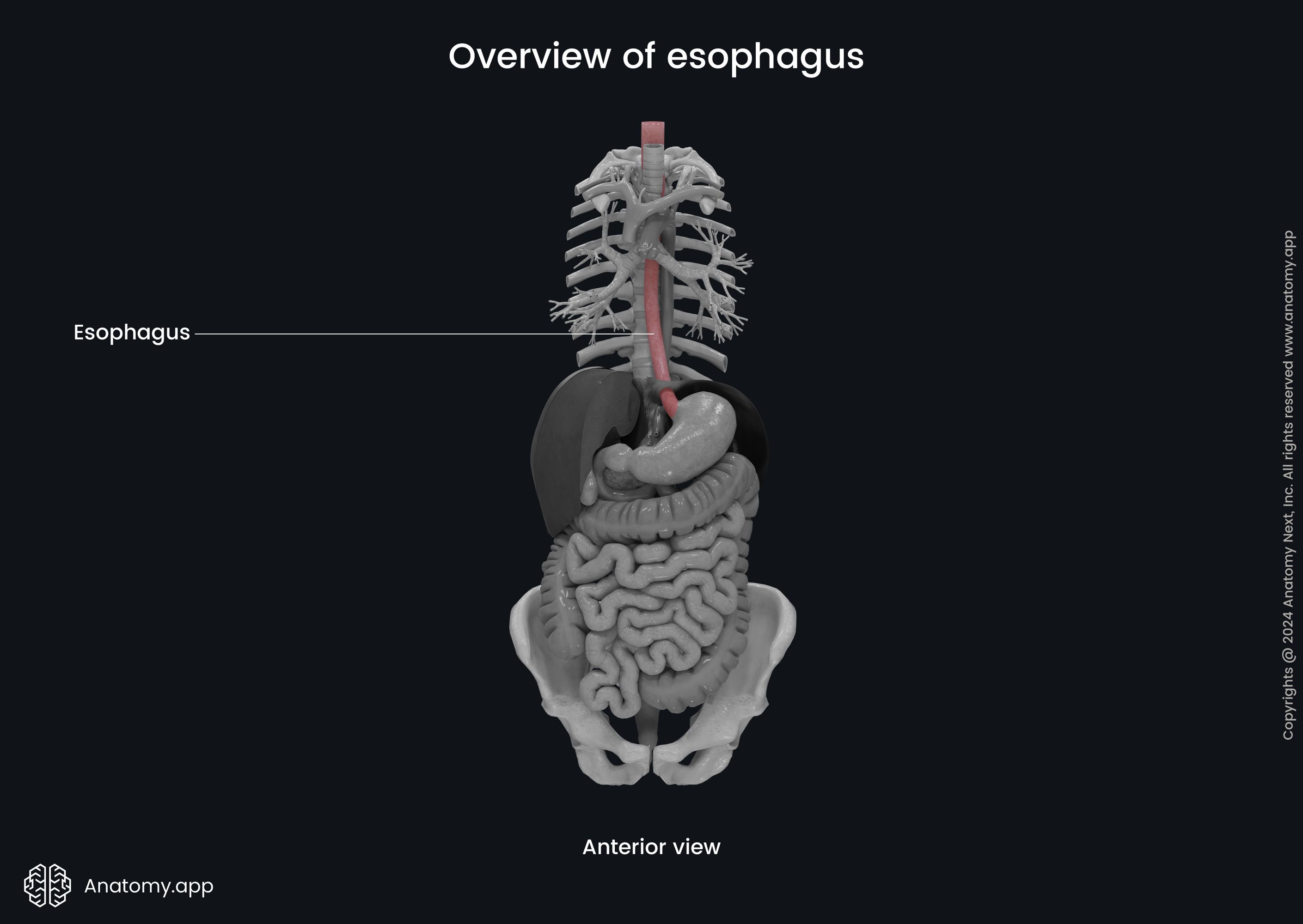
Esophagus
The esophagus (Latin: oesophagus) is a fibromuscular tube-shaped and elongated organ of the digestive system, part of the gastrointestinal tract connecting the pharynx with the stomach. The esophagus provides transport of ingested food and liquids to lower parts of the digestive tract through peristaltic muscle contractions.
Esopahgus anatomy
The esophagus is approximately 10 inches (25 cm) long and 1 inch (2 cm) in diameter in adults. It starts at the inferior edge of cricoid cartilage at the level of the sixth cervical vertebra (C6) as the continuation of the laryngopharynx, which is above it and is the distal part of the pharynx. The esophagus passes through the neck region and thorax, and enters the abdominal cavity.
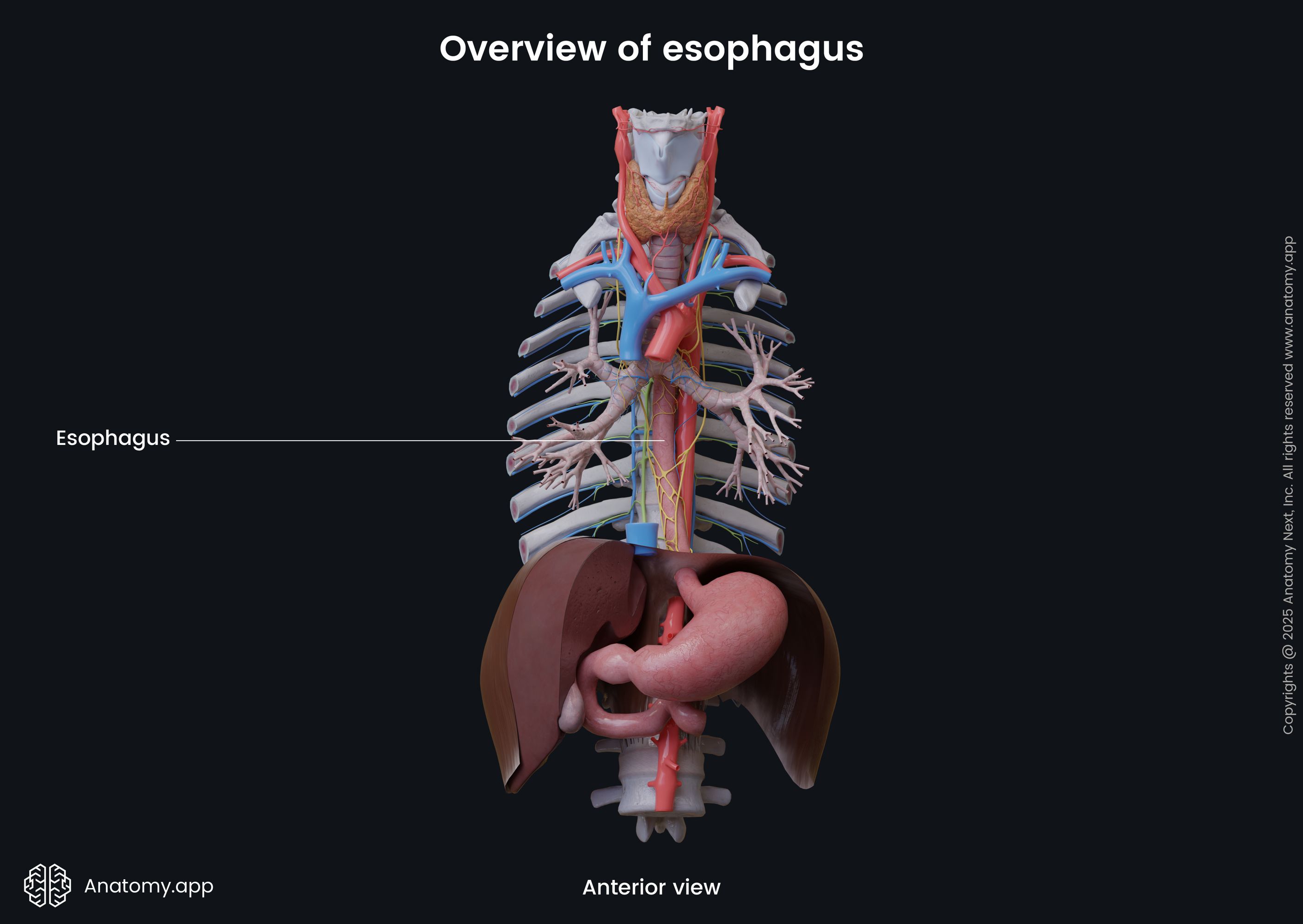
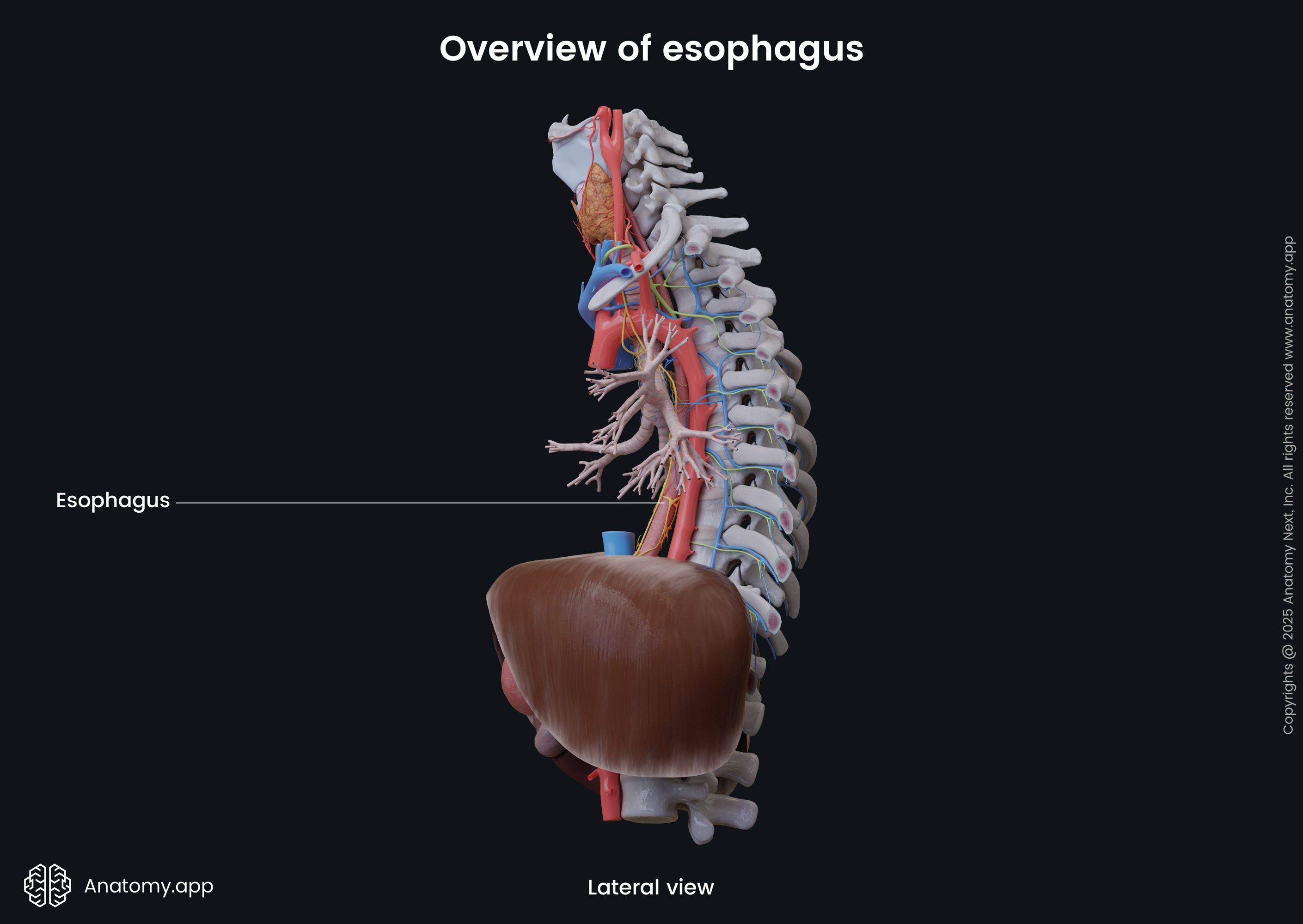
In the thoracic cavity, the esophagus is located in the superior and posterior mediastinum. It exits the thoracic cavity and enters the abdominal cavity by passing through the diaphragm. The esophagus ends at the eleventh thoracic (T11) vertebral level and passes into the stomach through the cardiac orifice of the stomach.
Esophagus parts
The esophagus is divided in three parts based on topographic location:
- Cervical part
- Thoracic part
- Abdominal part
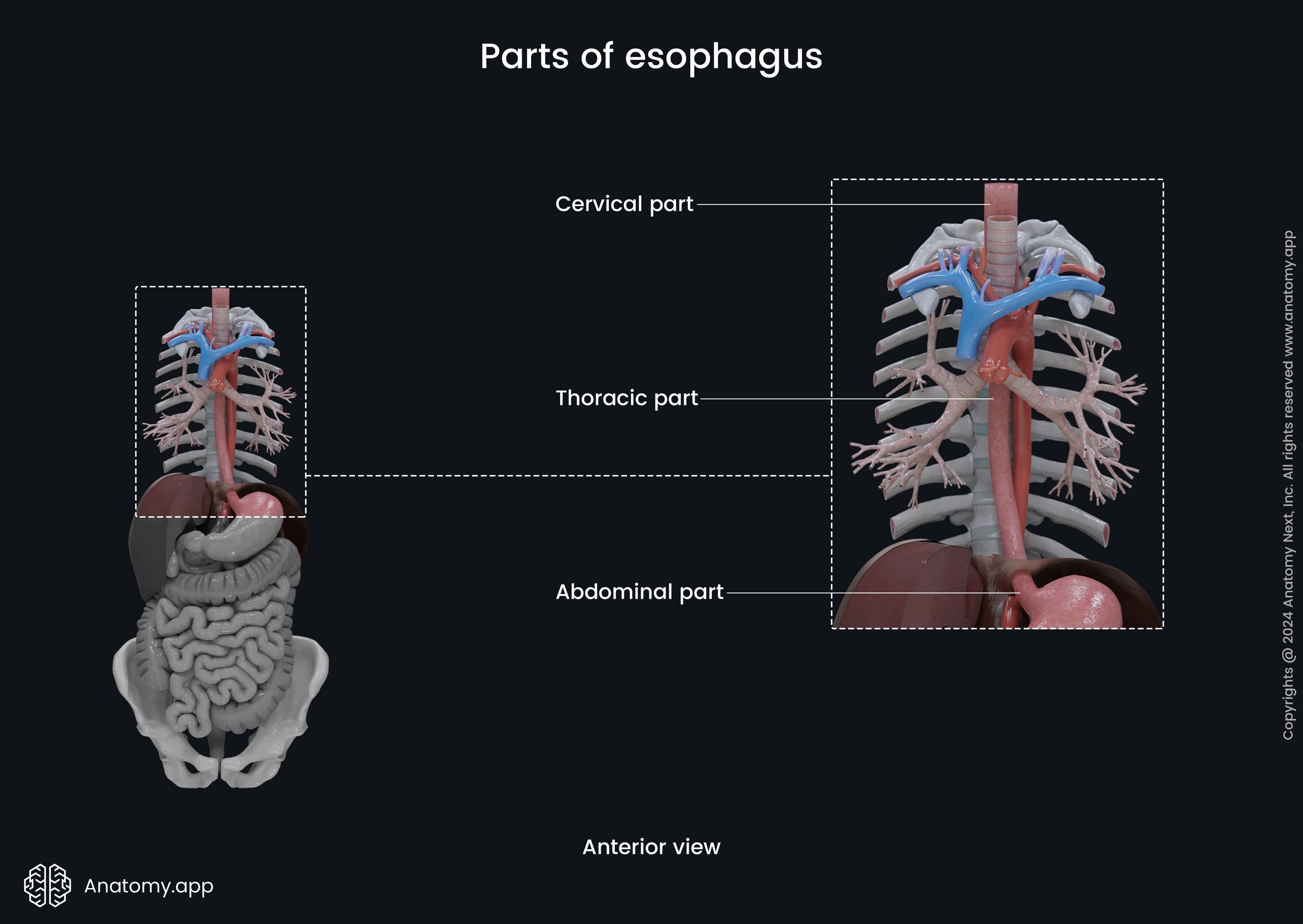
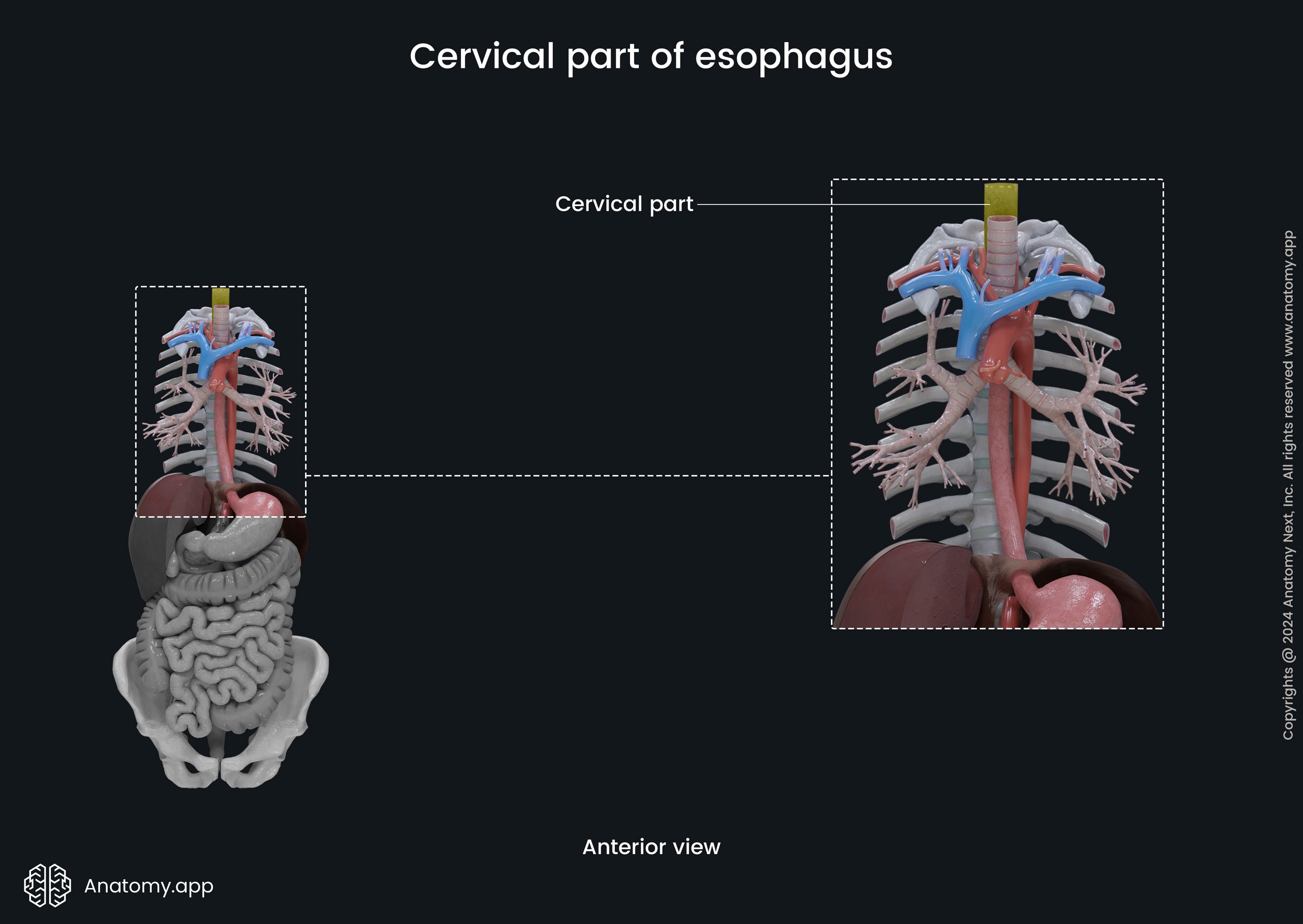
Cervical part of esophagus
The cervical part of the esophagus extends from the esophageal opening at the inferior border of the cricoid cartilage to the thoracic inlet, also known as the superior thoracic aperture at the level of the first thoracic vertebra (T1). Anterior to it is the jugular notch of the sternum. The cervical part is around 2 inches (5 cm) long.
Relations of cervical part
The cervical part is a continuation of the lowest part of the pharynx (hypopharynx). It passes behind the trachea and is connected with it through loose connective and muscular tissue. Posterior to the cervical part of the esophagus are the bodies of the sixth to seventh cervical (C6 - C7) and first thoracic (T1) vertebrae, which are connected to the esophagus with the help of the prevertebral fascia and muscles.
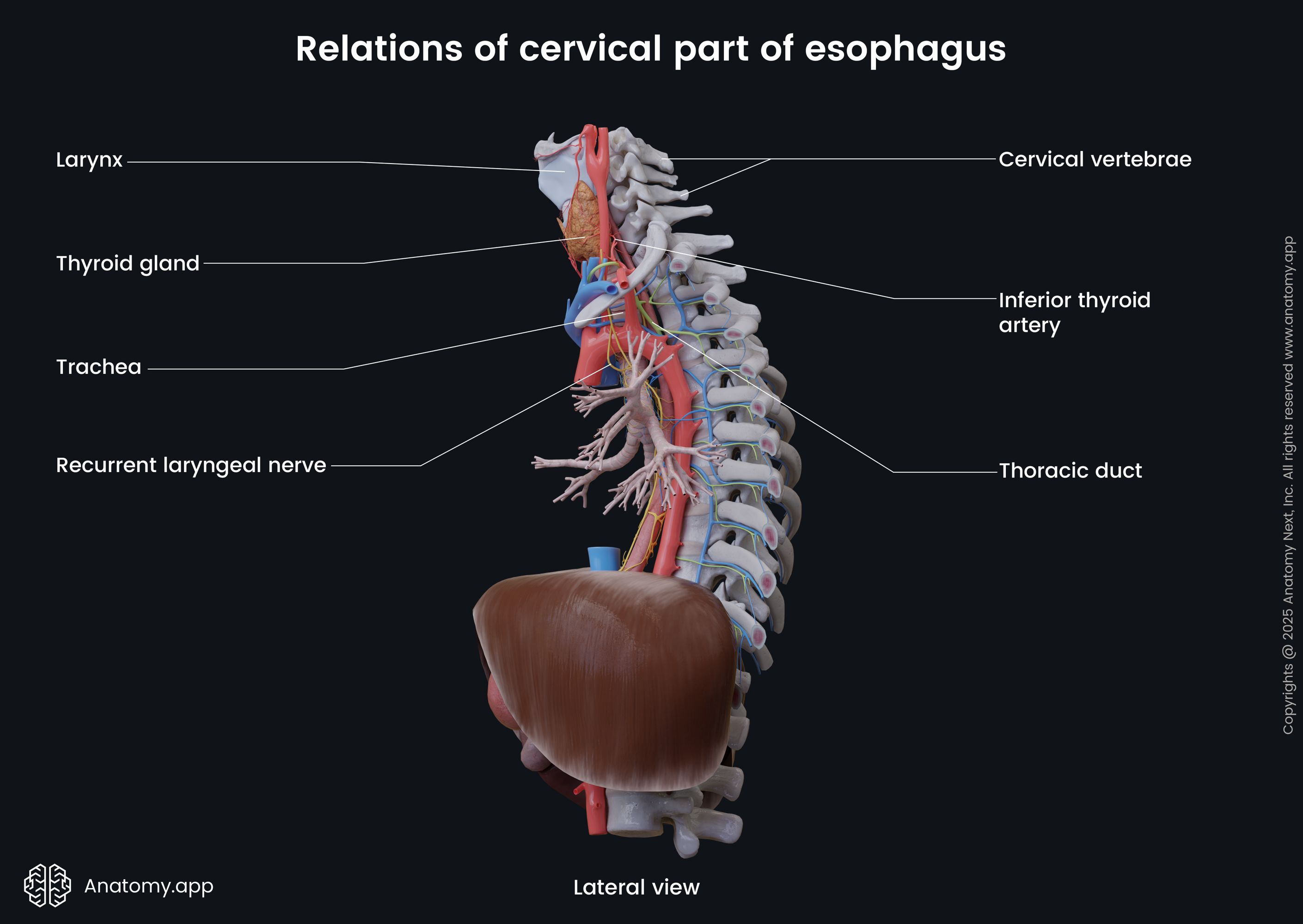
At the sixth cervical (C6) vertebral level, the thoracic duct lies on the left side of the cervical part of the esophagus. Close to the thoracic part anterolaterally to the esophagus passes the carotid sheath and lie the lobes of the thyroid gland. The inferior thyroid artery and recurrent laryngeal nerve also travel next to the cervical portion of the esophagus.
Thoracic part of esophagus
The thoracic part goes from the thoracic inlet and sternal notch of the sternum to the esophageal hiatus of the diaphragm. The thoracic portion is extends from the level of the first to the tenth thoracic vertebrae (T1 - T10). It is situated in the superior and posterior mediastinum. This part of the esophagus contains curves, as well as anatomical and physiological constrictions.
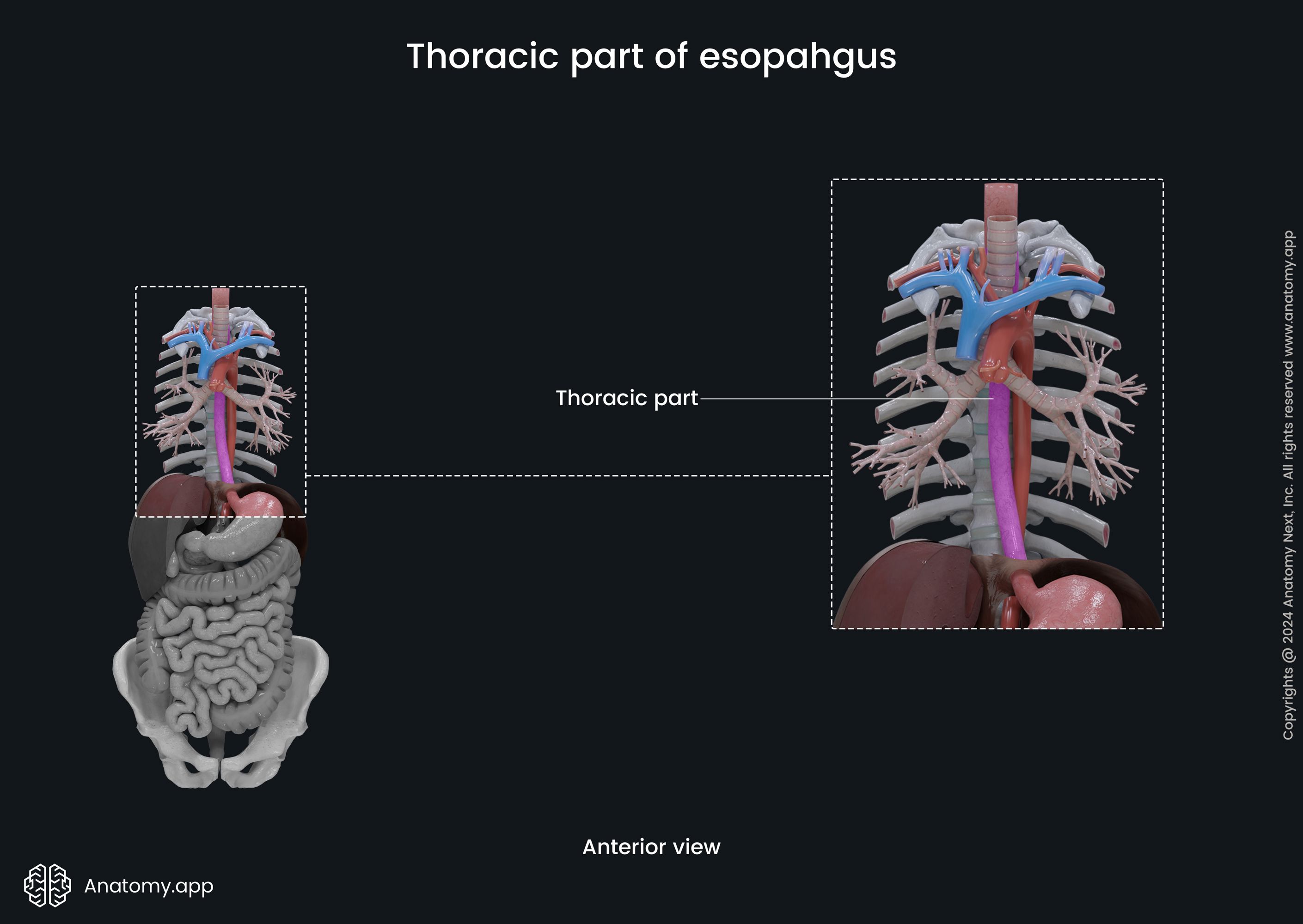
The upper thoracic part of the esophagus is located within the superior mediastinum of the thoracic cavity. It lies between the spine and the trachea. The lower thoracic part travels through the posterior mediastinum. The total length of the thoracic part of the esophagus is around 6 - 7 inches (17 - 19 cm).
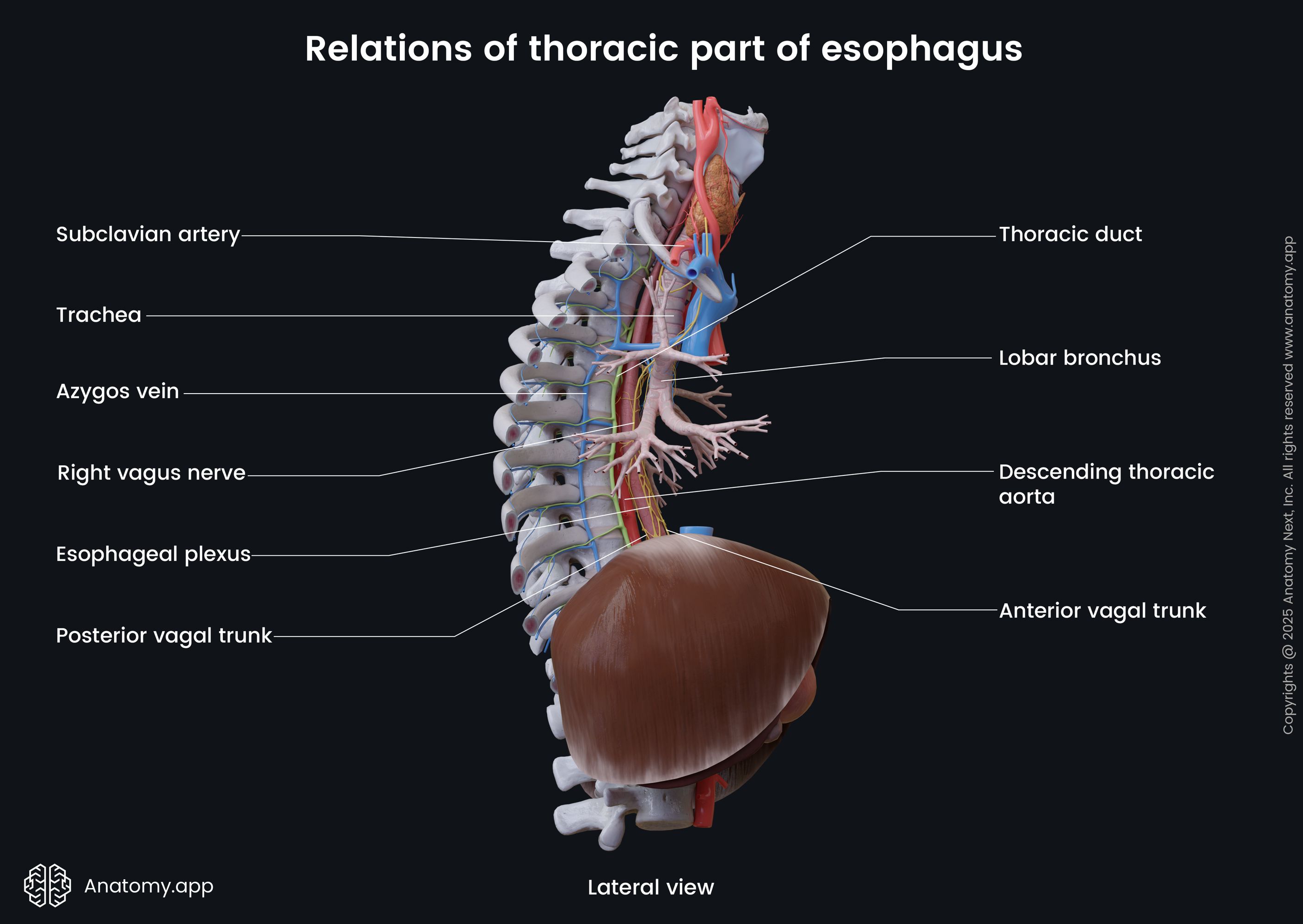
Relations of thoracic part
Anterior to the thoracic part are the trachea, left main bronchus, aortic arch, right pulmonary artery, esophageal plexus, pericardium, anterior vagal trunk, and left atrium of the heart. The thoracic part travels behind the aortic arch at the fourth thoracic (T4) to the fifth thoracic (T5) intervertebral disc level.
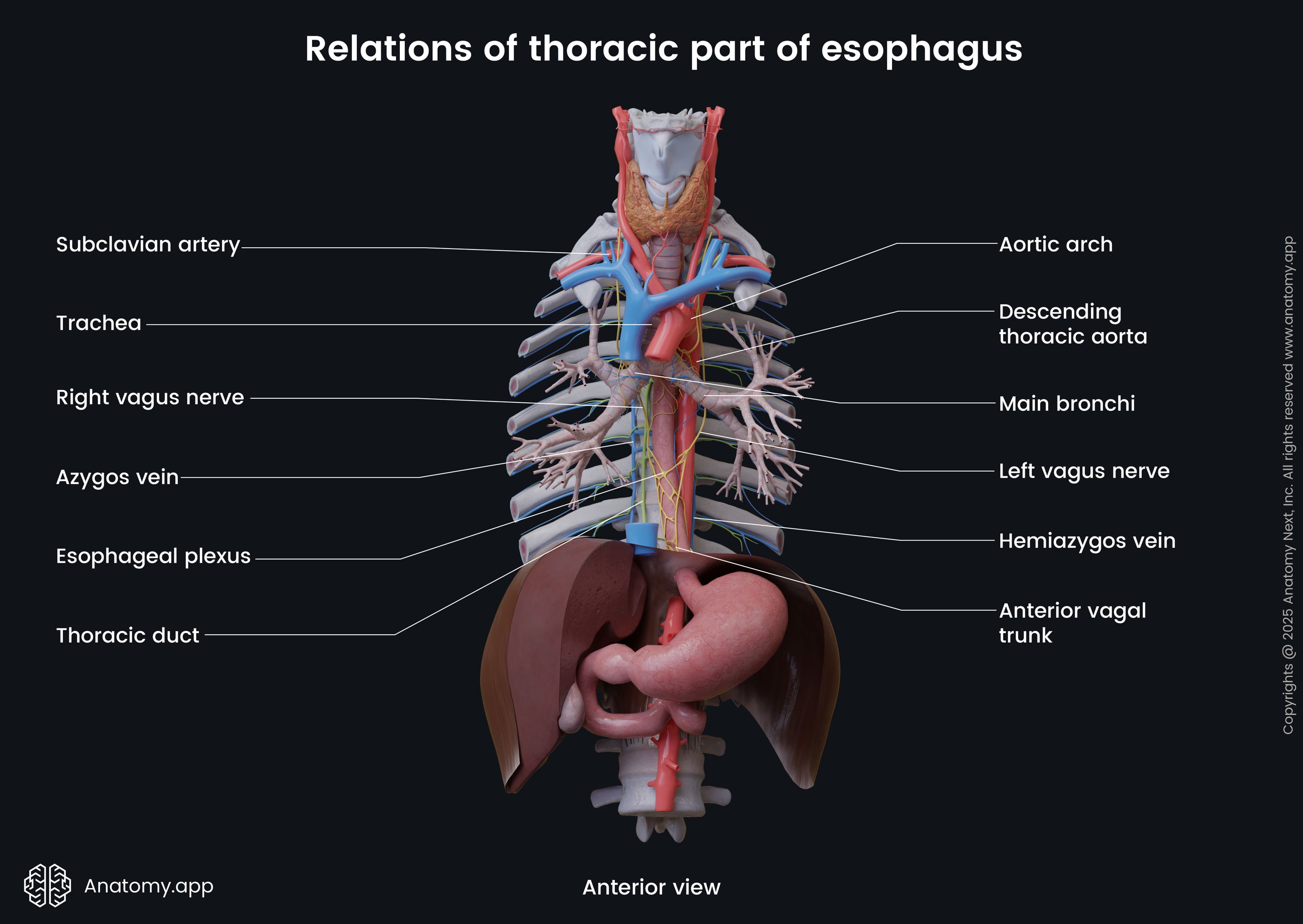
Posterior to thoracic part are located the thoracic vertebral bodies and thoracic duct, azygos and hemiazygos veins, posterior intercostal arteries, posterior vagal trunk, mediastinal pleura, descending thoracic aorta. At the eighth to ninth thoracic vertebral level (T8 - T9) the esophagus crosses the aorta.
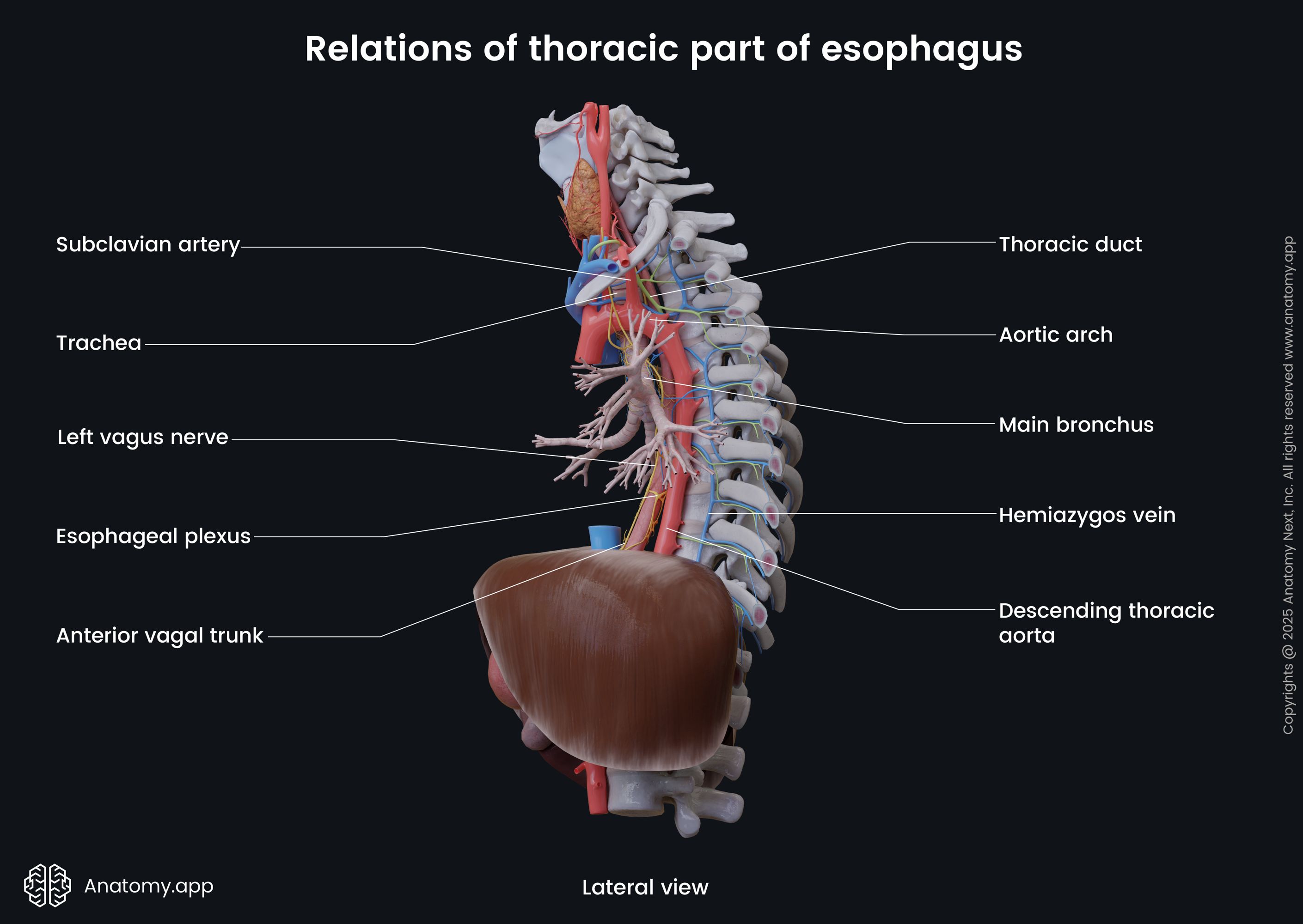
On the left side of the thoracic part of the esophagus, are the following structures: left subclavian artery, left vagus nerve (CN X), thoracic duct, aortic arch, left inferior laryngeal nerve, and the descending thoracic aorta. On the right side, are the mediastinal pleura, azygos vein, right vagus nerve (CN X), and the right main bronchus.
Abdominal part of esophagus
The abdominal part of the esophagus extends from the esophageal hiatus of the diaphragm to the cardiac orifice of the stomach. It is the shortest part of the esophagus - 0.4 to 1.2 inches (1 to 3 cm) long. The abdominal part of the esophagus is covered by the peritoneum.
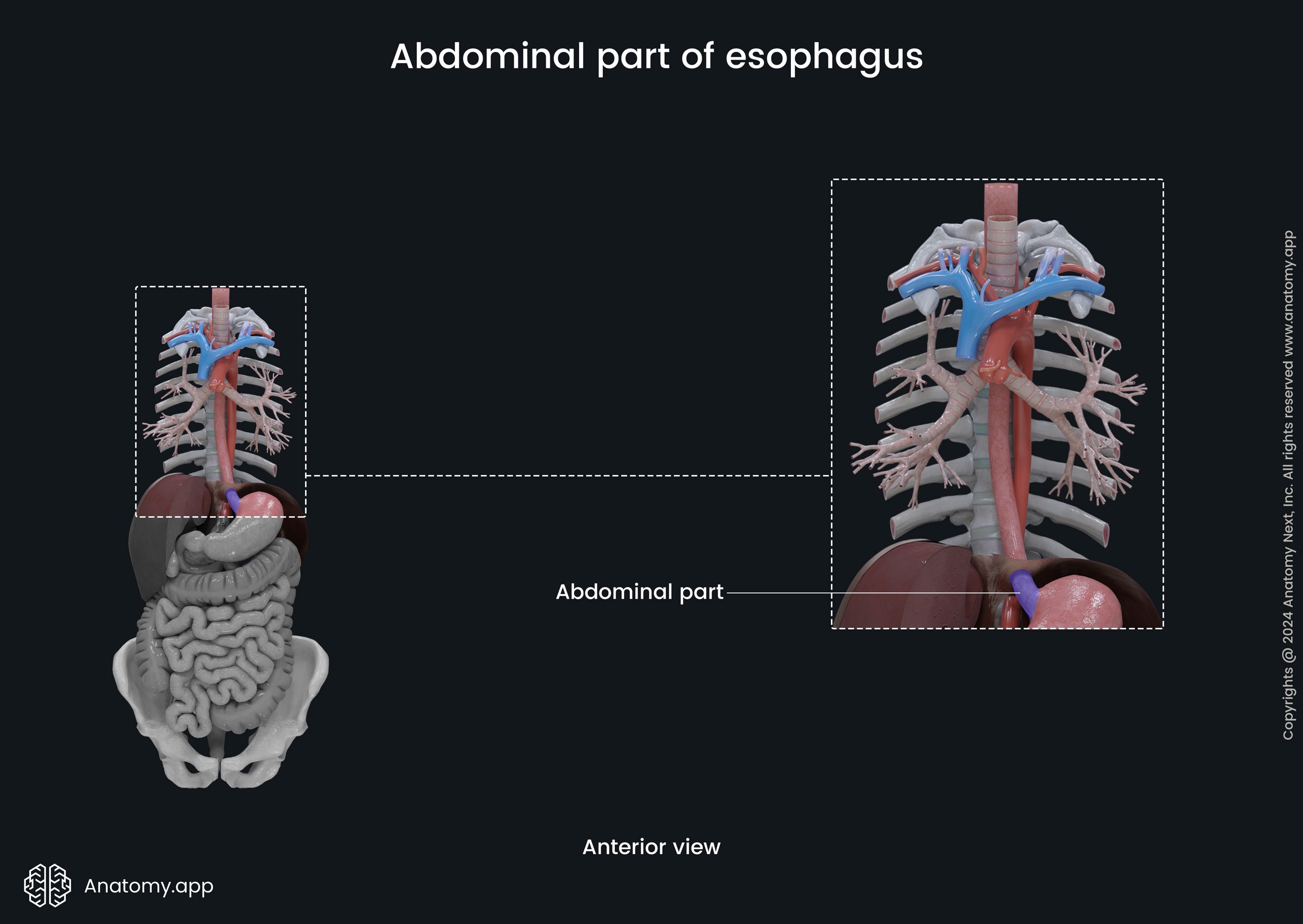
The esophagus goes through the diaphragm by passing through the esophageal hiatus formed by the muscular fibers of the right crus of the diaphragm at the tenth thoracic vertebral (T10) level. It reaches the cardiac orifice at the level of the eleventh thoracic vertebra (T11).
Relations of abdominal part
The abdominal esophagus is attachmed to the diaphragm via the phrenicoesophageal ligament formed by fibers of the pleura, subpleural fascia, transverse fascia of abdomen and peritoneum, and the phrenicoesophageal fascia.
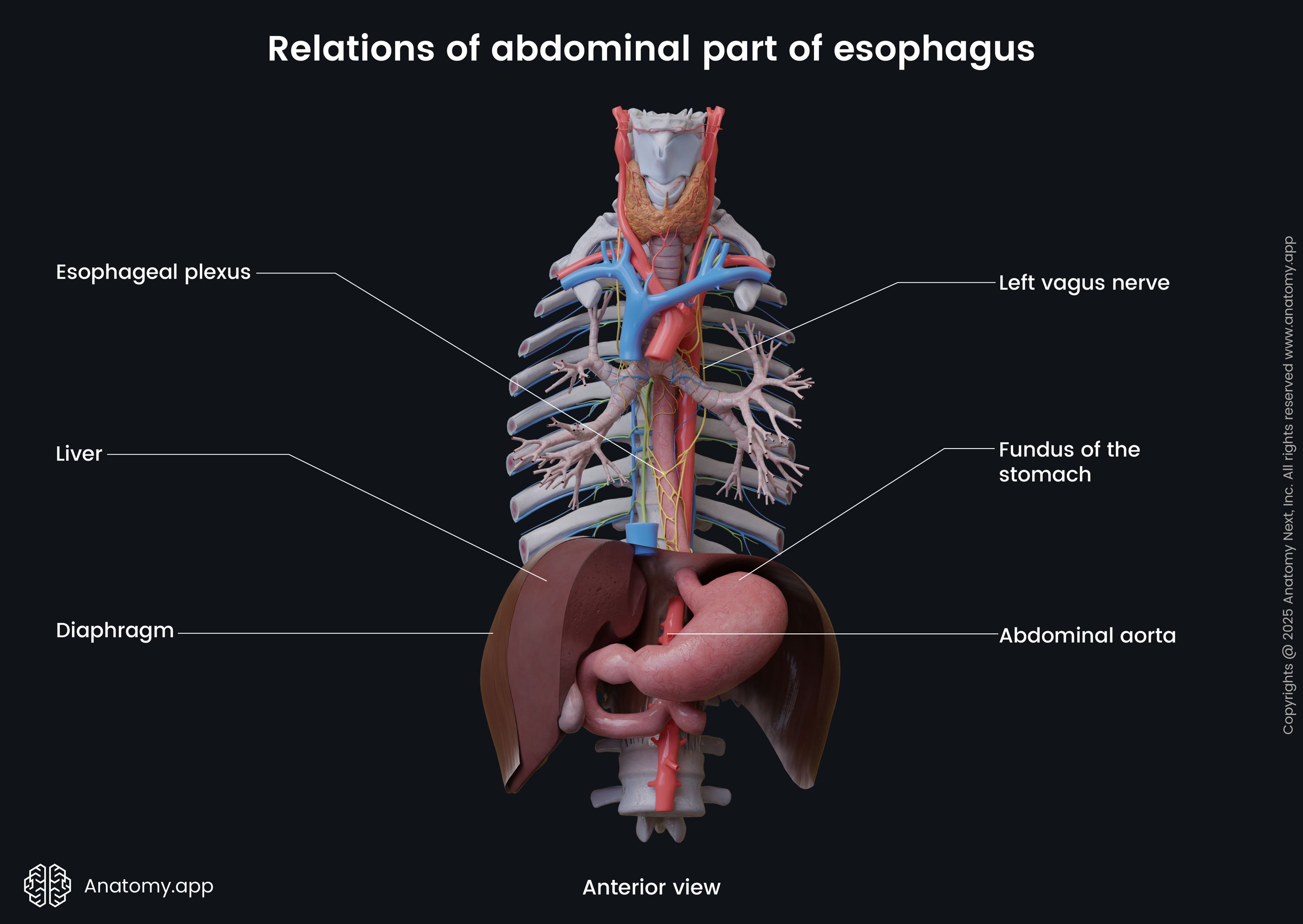
Anterior to the abdominal part of the esophagus are the liver, left vagus nerve (CN X), esophageal plexus, and the posterior surface of the heart. Posterior to it are the eleventh thoracic vertebral body (T11), right vagus nerve, both crura of the diaphragm, left inferior phrenic artery, and the abdominal aorta. On the right side lies the liver, but on the left - the fundus of the stomach.
Curves of esophagus
The esophagus has three slight curves in the coronal plane, where it deviates a little bit from the midline. It deviates to the left side in the neck part. But in the middle behind the left main bronchus - to the right side from the midline. At the end of the thoracic portion behind the pericardium, the esophagus deviates again to the left side. The curves give the esophagus the appearance of a reversed letter "S."
Constrictions of esophagus
The esophagus has four anatomical narrowings or constrictions:
- Pharyngoesophageal constriction - at the level of the esophageal opening, located at the sixth cervical vertebral level (C6); approximately 0.6 inches (1.5 cm) wide; corresponds to the location of the upper esophageal sphincter;
- Aortic constriction - located in the area where the esophagus is crossed by the aortic arch; located at the fourth thoracic vertebral level (T4); around 0.6 inches (1.5 - 1.6 cm) wide;
- Bronchial constriction - at the point where the esophagus crosses the left main bronchus at the fifth thoracic vertebra level (T5);
- Diaphragmatic (phrenic) constriction - at the level of the tenth thoracic vertebra (T10), where the esophagus passes through the esophageal hiatus of the diaphragm.
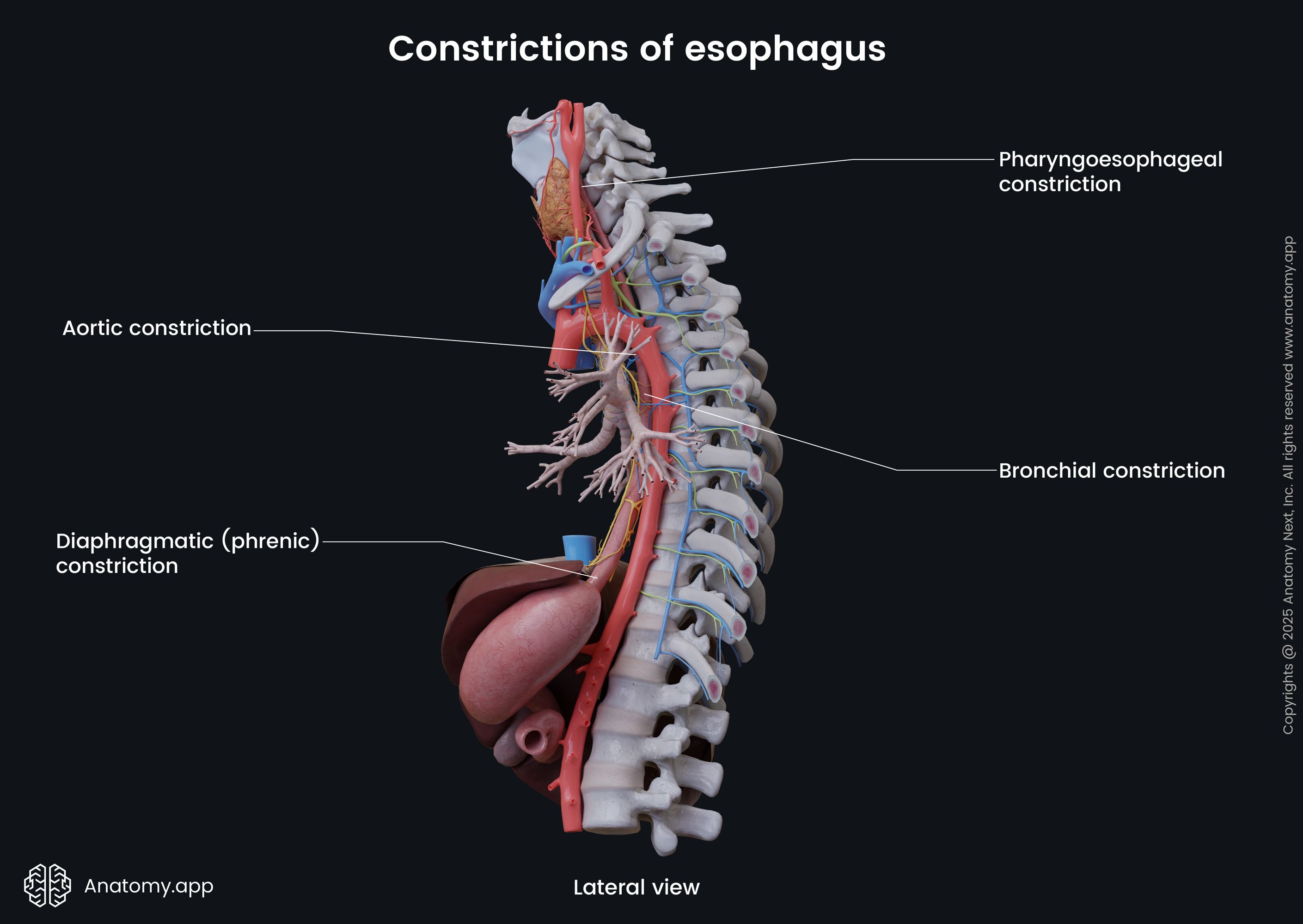
The esophagus may also have physiological narrowings. The first is below the bronchial constriction, and it develops when atrial dilatation is present. The second narrowing is at the point where the esophagus crosses the aorta at the eighth and ninth thoracic vertebral level (T8 - T9), and it happens in case of atherosclerosis affecting the aorta. The esophagus has one more physiological constriction at the level of the superior border of the sternum.
Esophageal sphincters
The esophagus has two sphincters located in its superior and inferior ends, preventing the backflow of the gastric acid - from the stomach back into the esophagus, as well as air passage to the stomach when digestion is not present. The two sphincters are known as the upper and lower esophageal sphincters.
Upper esophageal sphincter
The upper esophageal sphincter (also known as the inferior pharyngeal sphincter) is formed by striated (voluntary) muscle fibers, and it is an anatomical sphincter. It is located between the pharynx and esophagus. The junction is called the pharyngoesophageal junction. The fibers from the cricopharyngeus muscle form this sphincter with additional fibers from the inferior pharyngeal constrictor muscle. The upper sphincter prevents air from the airways going further into the digestive tract by staying constricted.
Lower esophageal sphincter
The lower esophageal sphincter is more physiological. It is made up from longitudinal and circular smooth muscle cells, the right crura of diaphragmatic muscle, and fibers from the phrenoesophageal ligament. The lower sphincter is located between the stomach and esophagus left to the midline at the eleventh thoracic vertebral level (T11). This sphincter is responsible for protecting the esophagus from reflux of the gastric content back up into the esophagus.
The place where the esophagus meets the stomach is called the gastroesophageal junction. At the site where the sphincter is located, the gastric mucosa changes the esophageal mucosa. Several anatomical features help the functioning of the lower sphincter. The esophagus has an acute angle where it meets the stomach. The mucosa contains prominent folds at the junction, which helps to constrict the esophagus. When positive intrabdominal pressure is present, the walls of the esophagus are in a compressed condition.
Esophagus histology
The wall of the esophagus is composed of four layers:
- Mucosa
- Submucosa
- Muscular layer (muscularis propria)
- Adventitia / serosa
Mucosa
The mucosa (or mucous membrane) of the esophagus is lined by non-keratinized stratified squamous epithelium. In the cardia part of the stomach, the mentioned epithelium changes into the simple columnar epithelium. The margin where it transforms is known as the Z line or the squamocolumnar junction, and it has an irregular zigzag shape.
The esophageal mucosa contains lamina propria, a loose connective tissue layer supporting the epithelium, and lamina muscularis mucosa, a muscular layer of the mucosa beneath the lamina propria. The mucosa also contains individual lymphatic aggregates.
Submucosa
The submucosa lies beneath the mucosa and contains mucus-producing esophageal glands, which lubricate the esophageal wall and facilitates the ingestion of the food bolus. The esophageal glands are acinotubular mucous glands.
In the region close to the pharynx, the glands are simpler in form. Glands of the abdominal esophagus closely resemble the cardiac glands of the stomach, and are called esophageal cardiac glands. The esophageal glands can also contain endocrine cells.
The submucosa also contains many blood vessels and lymphatics, nerve plexuses, and dense irregular connective tissue, including a relatively massive amount of elastic and collagen fibers. The nerve plexus located in the submucosa is also known as Meissner's plexus.
The mucous membrane and submucosa contain many muscle fibers allowing the esophageal folds to smoothen when swallowing the food bolus. The mucosa and submucosa create longitudinal folds or plicas, usually, seven to ten of them. This is the reason why the esophagus in cross-section looks star-shaped.
Muscular layer
The muscular layer (also called the muscularis propria) is very thick and has two sublayers. The outer or external is longitudinal, and the inner is circular. The thickest part of the layer is around the entrance to the stomach. Between the muscle cells is a significant amount of elastic fibers helping to move the hard and rough food particles through the esophagus.
In the muscular layer, striated skeletal muscles change into the smooth muscles. The upper one-third contains only striated (voluntary) muscles, the middle one-third has striated and smooth (involuntary) muscles, while the lower one-third contains only smooth muscle fibers. Between the outer longitudinal and inner circular muscle layers is a nerve plexus, called Auerbach's plexus.
Adventitia/serosa
The adventitia is formed by loose connective tissue covering the cervical and thoracic parts of the esophagus. The abdominal part is covered by the peritoneum instead of the adventitia. In this case, it is called serosa. The serosa faces the abdominal cavity and is lined by a single layer of squamous epithelial cells (mesothelium), which is supported by loose connective tissue.
Neurovascular supply of esophagus
Arterial blood supply
All parts of the esophagus receive arterial blood supply via esophageal branches arising from various arteries. The esophageal branches of the inferior thyroid artery (from the thyrocervical trunk) provide blood supply to the cervical part of the esophagus.
The thoracic part is supplied by the esophageal branches of the thoracic aorta and bronchial arteries. The abdominal part gets arterial blood supply from the left gastric artery - a branch of the celiac trunk. The left inferior phrenic artery that arises from abdominal aorta also supplies the abdominal esophagus.
Venous drainage
The cervical part of the esophagus is drained by the inferior thyroid veins carrying blood next to brachiocephalic veins that drain into the superior vena cava. The thoracic part is drained by the esophageal plexus to the esophageal veins and hemiazygos vein, which flows into the azygos venous system that carries venous blood to the superior vena cava. Also, the inferior thyroid, intercostal and bronchial veins aid in draining the middle part of the esophagus. The abdominal part is drained by the left gastric vein that carries venous blood to the portal venous system. It is also drained via the azygous vein.
Innervation
The esophagus is supplied by the autonomic nervous system, primarily via the sympathetic trunk (sympathetic fibers) and vagus nerve (CN X) (parasympathetic fibers).
The sympathetic fibers that participate in innervation of the esophagus arise from neurons located in the spinal cord segments T1 to T10 and pass through the cervical and thoracic ganglia of the sympathetic trunk. The parasympathetic fibers are supplied by the vagus nerve (CN X) and they originate from the nucleus ambiguous and dorsal nucleus of the vagus nerve (located in the medulla oblongata).
The visceral motor neurons from the dorsal motor nucleus act through connection with the esophageal myenteric nervous system and innervate the smooth muscles in the wall of the esophagus and the lower esophageal sphincter. The parasympathetic fibers stimulate secretion of the mucosal glands of the esophagus and initiate muscular contractions. The sympathetic and parasympathetic nervous systems regulate the glandular secretion of these glands.
The parasympathetic nerve supply comes from the vagus nerve (CN X) via the esophageal branches of the recurrent laryngeal nerve. These branches innervate the mucosa, glands, striated skeletal muscles of the upper one-third of the esophagus, and the upper esophageal sphincter. The sympathetic innervation of the cervical part of the esophagus is provided by nerves coming from the cervical ganglia of the sympathetic trunk.
The thoracic part of the esophagus (mucosa, glands, striated muscles) are innervated by the esophageal branches of the esophageal plexus. The parasympathetic fibers of the esophageal plexus are supplied by the vagus nerve (CN X), while the sympathetic fibers come from the thoracic ganglia of the sympathetic trunk.
The abdominal part of the esophagus is innervated by esophageal branches of the esophageal plexus and superior gastric plexus, also receiving fibers from the vagus nerve (CN X) and the sympathetic trunk.
Lymphatic drainage
The lymphatic drainage of the esophagus is provided by various lymph node groups. The lymph collected from the upper one-third of the esophagus drains into deep cervical lymph nodes. Lymph from the middle one-third drains into superior and posterior mediastinal nodes. And the lower one-third of the esophagus is drained by the celiac and left gastric lymph nodes.
Esopahgus functions
The primary function of the esophagus is to transport the food bolus from the pharynx to the stomach.
- The esophageal glands produce mucus, lubricating the bolus and helping in its transportation.
- The esophagus moves the food bolus by peristalsis - rhythmic wave-like muscle contractions and motion of circular muscular tissue. Contractions travel downwards from the superior to inferior parts of the esophagus, moving the bolus further in the direction of the stomach.
- The contractions of peristalsis are categorized into primary and secondary contractions. Primary peristalsis move the bolus, while secondary peristalsis clears the esophagus from any remaining food particles.
- The esophagus not only moves the food further inside the body, but it also helps to remove it from the body, in case of vomiting. This may be caused by various diseases or medical issues (for example, hyperemesis gravidarum or the morning sickness in pregnancy), or stimulation of gag reflex. Therefore, the esophagus also has a protective role.
References:
- Drake, R., Vogl, W., & Mitchell, A. (2019). Gray’s Anatomy for Students: With Student Consult Online Access (4th ed.). Elsevier.
- Gray, H., & Carter, H. (2021). Gray’s Anatomy (Leatherbound Classics) (Leatherbound Classic Collection) by F.R.S. Henry Gray (2011) Leather Bound (2010th Edition). Barnes & Noble.
- Moore, K.L., Dalley, A.F., Agur, A.M. (2018). Clinically Oriented Anatomy, 8th Edition, Lippincott Williams & Wilkins.